Prostate disease is one of the most common and insidious in men over 40. At first, patients may not even be aware of a problem, but over time, the symptoms are felt. If you do not consult a doctor in time, prostatitis becomes chronic and complications can arise. Depending on the severity, causes and nature of the course, several types of prostatitis are distinguished.
Types of prostatitis according to the form of its course:
- acute;
- chronic;
- latent.
What is prostatitis due to the occurrence of:
- herpetic;
- bacterial;
- calculous;
- stagnant;
- contagious;
- purulent;
- chlamydia;
- fungal;
- gonorrheal;
- fibrous.
Classification
Faced with such an unpleasant disease of the genitourinary system as inflammation of the prostate gland, many men wonder why they have prostatitis.
Understanding the etiology of the disease helps in accurate diagnosis and effective prevention.
From the shape of the stream
According to the form of the course, prostatitis is divided into acute, chronic and latent, among which catarrhal, follicular, parenchymal (purulent) are distinguished.
There are the following forms of the disease:
- With catarrhal prostatitis in the male body, there is a disturbance of urination and discomfort in the pubic region. This is the most common type of acute prostatitis.
- Follicular prostatitis is characterized by symptoms such as pain in the groin or anus, fever, and severe urinary disorders (dysuria). In a more advanced form, when the patient postpones the visit to the doctor, sharp pains and urinary retention occur during urination.
- Parenchymal prostatitis - an abscess with purulent contents is formed in the body of the prostate gland. In this case, fever occurs, sharp pains appear with a frequent need to urinate. The temperature rises to 39-40 ° C, the act of defecation becomes almost impossible.
Acute prostatitis
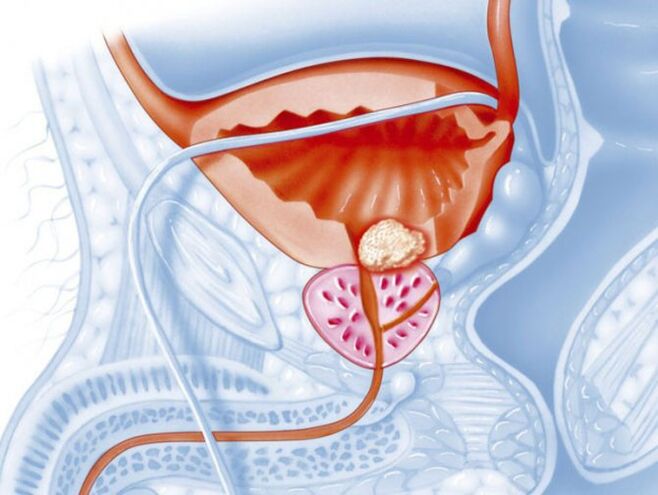
Acute prostatitis is a condition in which there is inflammation of the prostate gland, which manifests itself in a short time and is characterized by various symptoms. Swelling of the gland occurs, provoked by the negative effects of pathogenic microflora. Pathogenic bacteria disrupt tissue integrity, causing permanent discomfort in the pelvic region, even at rest.
There are several predominant routes for infection to enter the prostate gland:
- with inflammation of the rectum - the lymphogenous path;
- after infectious diseases - hematogenous;
- directly through the urethra - canalicular.
Excessive accumulation of contents in the prostate gland creates excellent conditions for the growth of bacteria, which causes various complications:
- abscess;
- BPH;
- prostate cancer;
- loss of power;
- infertility.
Symptoms of prostatitis are so painful that the patient is forced to urgently consult a doctor for help. If you don't do it in time, prostatitis will turn into a chronic form, which is much more difficult to cure. Antibiotic therapy in combination with drugs that strengthen the immune system effectively fights the disease.
Chronic prostatitis
Symptoms of chronic prostatitis are usually found against the background of congestion in the prostate gland, resulting from an untreated disease in an acute form. It usually occurs in men over 50 who have not sought help and have self-medicated. Many of them have developed complications due to concomitant diseases. In addition, at this age, not everyone is sexually active enough, as a result of which the secret thickens and stagnates in the prostate, which leads to dysfunction. Interrupted intercourse also causes fluid stagnation. According to modern research, around 40% of people who experience chronic prostatitis symptoms experience erection problems.
Chronic prostatitis, as a rule, has mild symptoms that appear only during an exacerbation. Patients notice dull pain in the groin area, which increases after physical exertion and at the end of the day. The pain often radiates to the lower back, scrotum, and perineum. Frequent urination is noted, especially at night, the flow is intermittent, spills crooked.
Sexual intercourse becomes shorter, incomplete erection is noted, sometimes there is pain in the glans penis. Infertility is usually found in people with chronic prostatitis; impotence at this stage of the disease is practically non-existent. Sometimes there is a change in the color of the genitals, due to improper blood circulation, they turn purple.
Each of the symptoms of prostatitis gets worse if left untreated. The condition is similar to the manifestations in the acute course of the disease. Weakening of the immune system, stress, abandonment of diet, bad habits - all this leads to an exacerbation and deterioration of the condition.
Often the chronic form leads to the appearance of symptoms of diseases such as cystitis, kidney disease and adenoma. Increases the risk of urolithiasis and the formation of a malignant tumor. Often the pathological process is almost asymptomatic and is discovered almost by chance during laboratory tests associated with another disease.
Due to the occurrence
There are many reasons that provoke the development of prostatitis of infectious and non-infectious etiology, as well as predisposing factors. Due to the occurrence, the following types of prostatitis are distinguished:
- bacterial;
- calculous;
- stagnant;
- contagious;
- purulent.
A sedentary lifestyle, frequent hypothermia, rare sexual activity, interrupted sexual intercourse, smoking, alcohol abuse, stressful situations - all these circumstances affect the stagnation of secretions in the vessels of the prostate gland and in the vessels located next to it. Prostatitis is classified into several forms, depending on the reasons for its occurrence.
Bacterial prostatitis
Bacterial prostatitis is caused by bacteria that enter the prostate gland in various ways. It can be a type of bacteria or a group of them. The disease can be triggered by:
- mushroom;
- gonococci;
- Koch's wand;
- chlamydia;
- different types of bacteria at the same time.
The inflammatory process is most often associated with the penetration of bacteria into the prostate gland caused by sexually transmitted diseases. Promiscuous sex with frequent changes of partners and without the use of protective means leads to diseases such as gonorrhea, chlamydia, fungal infections. In addition, the development of pathology is facilitated by a decrease in immunity due to a violation of the regime of work and rest. Even bad habits, such as smoking, drinking alcohol, a sedentary lifestyle, etc. , They reduce immunity.
The most obvious symptoms accompanying bacterial-type prostatitis include burning, pain, and cloudy discharge when urinating. The smell of urine is unpleasant. General symptoms accompanying intoxication are observed: dizziness, weakness, nausea, fever. Pain is noted during ejaculation and sometimes blood is present. With chronic bacterial prostatitis, urination becomes more frequent, a yellowish or greenish discharge from the penis appears.
Calcareous prostatitis
With calcareous prostatitis, stones form in the ducts of the prostate gland. This form of the disease is very complex and is accompanied by severe pain. The conglomerates are of various origins: phosphates, oxalates, with a predominance of calcium and proteins.
There are two reasons for the presence of stones in the ducts: the stagnation of the contents of the gland and the passing of urine into the prostate.
Stagnation is associated with various factors that interfere with the normal outflow of secreted fluid. Prolonged sexual abstinence, hyperplasia, the presence of a tumor that closes the ducts and a sedentary lifestyle lead to stagnation of secretions and disruption of the vascular and lymphatic systems.

The throwing of urine is triggered by a malfunction of the sphincter, which relaxes, and urine flows both outside and inside. The presence of stones and sand in the bladder contributes to the development of stones in the ducts of the prostate. They enter with urine, settle and continue their growth, eventually reducing the outlet. Injury to the genital organs and surgery can lead to sphincter dysfunction.
At first, the calcareous form of prostatitis is asymptomatic, as the stones grow, the symptoms appear and increase. There is pain in the lower abdomen or scrotum, which radiates to the buttocks and lower back. Pain at rest is not observed and occurs only during physical exertion, the act of defecation and urination, as well as during intercourse and when walking.
Large stones with sharp edges during their movement injure the canal, which leads not only to pain, but also to the release of blood in the urine and ejaculate. Stone wounds can easily become infected and then calcareous prostatitis will turn into infectious.
After about a month, with calcareous prostatitis, the work of the whole body is stopped, a person feels unwell, experiences insomnia, increased fatigue and irritability.
In advanced stages of calcareous prostatitis, after a comprehensive diagnostic examination, a medicine is prescribed and surgical treatment is performed to remove conglomerates.
Congestive prostatitis
The stagnant appearance of prostatitis occurs due to a delay in secretion in the prostate gland. Most often, such problems are observed in men with sedentary work, who are not involved in sports. As a result of hypodynamia, there is a violation of blood circulation in the pelvic organs, the prostate suffers from insufficient supply of oxygen and nutrients, stagnation and inflammation occur. If nothing is done, the disease becomes chronic and causes great discomfort.
Congestive prostatitis causes an irregular sex life or its complete absence. In this case, men should independently release the gland from secretion, but do not overdo it, as regular masturbation can harm due to incomplete ejaculation. Many spouses have found on their own a way to prevent pregnancy such as a broken relationship. It also leads to incomplete ejaculation and inflammation.

Sometimes hypothermia or varicose vein disease becomes a provoking factor. Abnormalities in the structure of the prostate gland can also cause stagnation. Regular overheating of the pelvic region and constant constipation negatively affect the production of secretions. Depending on the factors provoking the disease, several types of congestive prostatitis are distinguished.
- Venous prostatitis. It happens in people with varicose veins of the lower extremities. In this disease, all organs of the small pelvis are affected due to improper circulation.
- Congestive. It develops with partial emptying of the prostate gland. The gradual overflow leads to stagnation.
- Chronic. It develops when the wrong lifestyle has become a habit. If nothing is done to change the situation, the disease becomes chronic. More often it happens in single men suffering from obesity, already in adulthood, when the anamnesis is burdened by concomitant diseases. At this stage, the prostate is often enlarged, which is easy to determine on examination.
- Contagious. It joins the already existing inflammation of the prostate when the infection enters the genitourinary system.
The manifested symptoms of prostatitis are caused by difficulty urinating, pain in the groin, tension during bowel movements and weakening of sexual activity. As a result of these symptoms, with stagnant types of prostatitis, poor health, irritability develops, working capacity decreases, and sleep is disturbed.
Infectious prostatitis
Microorganisms that can provoke the appearance of signs of acute prostatitis include Escherichia coli, Staphylococcus aureus, Proteus, Eltirococcus, Klebsiella. There are bacteria that are constantly in the body, but in a dormant state they do not lead to inflammatory processes. When it enters through the urethra on the mucous membrane of the prostate gland, the process of development and reproduction of microorganisms begins, as a result of which inflammation develops. Indiscriminate and unprotected sex also allows harmful bacteria to enter the body.
Typical symptoms are pain in the scrotum, perineum, lower abdomen, lower back, pain and burning sensation in the small pelvis. Difficulty urinating, acute urinary retention occurs. In addition to the listed symptoms accompanying an infectious type of prostatitis, constipation, discharge from the urethra, hemospermia, and pain during ejaculation may occur.
This is a dangerous disease that, even in the early stages, is able to provoke an infection of a sexual partner, lead to general blood poisoning or the development of pyelonephritis and cystitis.
Purulent prostatitis
Purulent prostatitis usually develops when a bacterial infection enters the prostate. The disease manifests itself in four stages.
- Catarrhal. It develops after suffering from acute respiratory viral infections, tonsillitis, flu. Purulent contents are present in the urine. There is a burning sensation when the bladder is empty. Patients notice a weakening of potency. The process that accompanies this type of prostatitis involves the superficial tissues of the prostate.
- Focal. The process extends to the glandular tissue. The ducts swell, the outflow is disturbed. The gland increases in size due to the accumulation of pus in it, which is excreted in the urine. Body temperature rises.
- Parenchymal. Connective tissue is involved in the process, edema becomes even greater, the temperature can reach 40 ° C. A crackling pain in the anus torments, a false urge to defecate is felt.
- Abscessive. The most insidious form of prostatitis. The temperature is severely confused, there is an abundant presence of pus and intolerable pain. This stage can be complicated by peritonitis and is fraught with death.
Purulent prostatitis can be complicated by symptoms and diseases such as paraproctitis, paracystitis, abscess, sepsis. Usually, these pathologies are treated surgically and involve the removal of purulent sacs.
Diagnostics
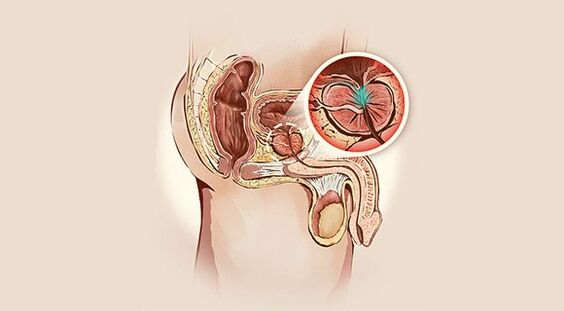
Diagnosis of types of prostatitis is not particularly difficult and begins with the collection of anamnesis, which helps to more accurately understand the picture of the disease. Then a rectal examination is performed, during which the size of the gland is determined, the nature of the pain is established, the presence of edema and seals is revealed.
To make a correct diagnosis, laboratory tests are prescribed:
- Urine analysis;
- urine culture with an AB sensitivity test;
- general blood test;
- analysis of prostate secretion;
- blood chemistry;
- rectal examination.
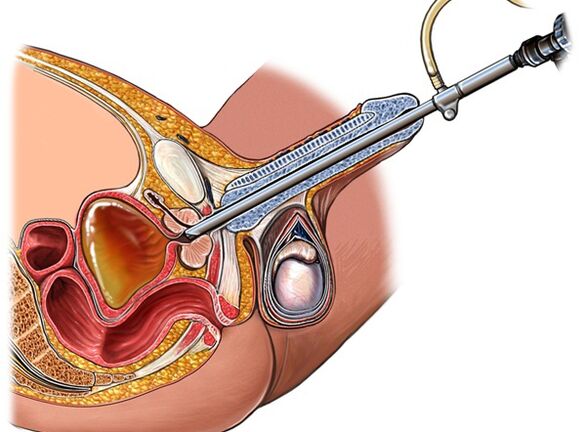
Additional diagnostics includes instrumental research methods. First of all, ultrasound is performed, if necessary, additional MRI and TRUS are prescribed. Relatively recently, a new method of PET examination has appeared, which is considered the most informative.
Treat inflammation
Urologists treat all types of prostatitis. Traditional methods are good, but only in conjunction with medical prescriptions and with the permission of the attending physician.
First you need to find out the cause of the disease, and only then can you carry out post-symptomatic treatment.
- Active antibiotic therapy helps cure prostatitis. Parenteral antibiotics are the most effective.
- With a pronounced pain syndrome, painkillers and diuretics are indicated.
- For constipation, laxatives are prescribed.
- With severe pain and difficulty urinating, novocaine blockade is placed.
- The course of vitamin therapy and immunocorrectors is shown.
- It is worth adhering to a special diet that excludes spicy, salty and smoked dishes.
- Bed rest is prescribed.
From local procedures, sitz baths with water are shown, the temperature of which is two degrees higher than body temperature. Enemas are made with a herbal decoction of anti-inflammatory herbs with the addition of 1% anesthetic, while the contents are slowly injected into the intestine and left there as long as the patient can resist.
Physiotherapeutic treatment also has a beneficial effect on the restoration of prostate function. Prostate massage with acute prostatitis is prohibited, but in the chronic form it is recommended. To restore metabolism, normal blood circulation and relieve edema, UHF and microwave are prescribed.
With prolonged urinary retention, a catheter is inserted. At some stages of the development of the disease, surgical treatment is indicated to open the purulent sacs with the installation of drainage.
Treatment of acute prostatitis takes from a few weeks to a month. A favorable result is usually observed. If the disease has become more complicated or has moved on to a chronic stage, the process will be difficult, long, and may take several months.
During the treatment, the limitation of sexual activity and the use of personal protective equipment are indicated.
A physiotherapy medical apparatus helps cure prostatitis. Effectively eliminates the symptoms of prostatitis, is able to restore reduced sexual activity, relieve pain, relieve swelling and inflammation. The device can be used at home for both treatment and prevention of diseases of the pelvic organs.
The device relieves muscle tension, improves sperm production, strengthens blood vessels and prevents the development of other possible diseases in the small pelvis. The device, with which prostatitis in men is treated, is easy to use, equipped with a regulator of the heating and vibration modes, and is powered by a network. The compact size allows you to use the device in any conditions.
How to prevent the development of the disease?
Prevention of various types of prostatitis, like any other disease, is a healthy lifestyle, without bad habits and a balanced diet. If you've been diagnosed with prostatitis, exercise shouldn't be neglected. For any nidus of inflammation that has occurred, a doctor should be consulted immediately to eliminate the cause and prevent the infection from entering other organs.
You should lead a decent lifestyle, have regular sex with a regular partner. It is important not to forget about personal hygiene of the genitals and not to neglect regular preventive examinations by a urologist. If a man knows what prostatitis can be and at the same time leads a passive lifestyle, it is necessary to perform exercises to prevent the appearance of congestion in the small pelvis.
Let's summarize
Depending on the causes and features of the course, acute and chronic types of prostatitis are diagnosed. Chronic pelvic pain syndrome belongs to a separate group. Acute prostatitis is characterized by clinical manifestations such as chills, fever and pain. The chronic form may not manifest itself in any way or has a mild image - a violation of urination, aching pain in the pelvic area, which, with the development of complications, can lead to impotence and loss of fertility.
Acute prostatitis develops suddenly and is easily diagnosed. Conversely, chronic prostatitis proceeds in waves, alternating periods of remission and exacerbation. In a chronic course, the identification of pathogenic microbes can cause some difficulties. Foci of infection occurring in the genitourinary system provoke complications in the form of diseases of the organs that are anatomically adjacent to the prostate gland. Depending on which prostatitis was diagnosed, the urologist prescribes a differentiated treatment regimen.































